Defeating the Stigma: Normalizing At-Home Testing and Treatment for STIs
At-home STI testing companies are normalizing testing and treatment by offering convenient, affordable, and private testing for STIs without visiting a doctor's office or clinic and providing discreet online consultations and treatment options.

Source: Adobe Stock
- Over the years, sexually transmitted infection (STI) testing and treatment have evolved from traditional methods requiring healthcare providers visits to more convenient and accessible options such as at-home testing kits and telemedicine consultations. Due to advances in medicine, more effective treatment options are available to reduce the duration and intensity of treatment for some STIs. Still, stigma and a lack of education about STIs continue to be obstacles to widespread testing and treatment for many, said Daphne Chen, MBA, Co-Founder at TBD Health, in an interview with LifeSciencesIntelligence.
“Unfortunately, there are a lot of structural challenges in seeking STI testing,” noted Chen. “STI testing is one the most stigmatized healthcare services out there, and the associated stigma deters people from pursuing necessary care and treatment.”
Because sex is often considered a private matter and is not discussed openly in many cultures, this leads to a lack of education and awareness about sexual health, and unfortunately, misconceptions and myths about sexual health — such as the idea that only promiscuous people get STIs — can contribute to stigma and shame.
A 2021 study published in the International Journal of Environmental Research and Public Health found that the shame and social disapproval associated with sexually transmitted diseases (STDs) can deter people from undergoing necessary testing.
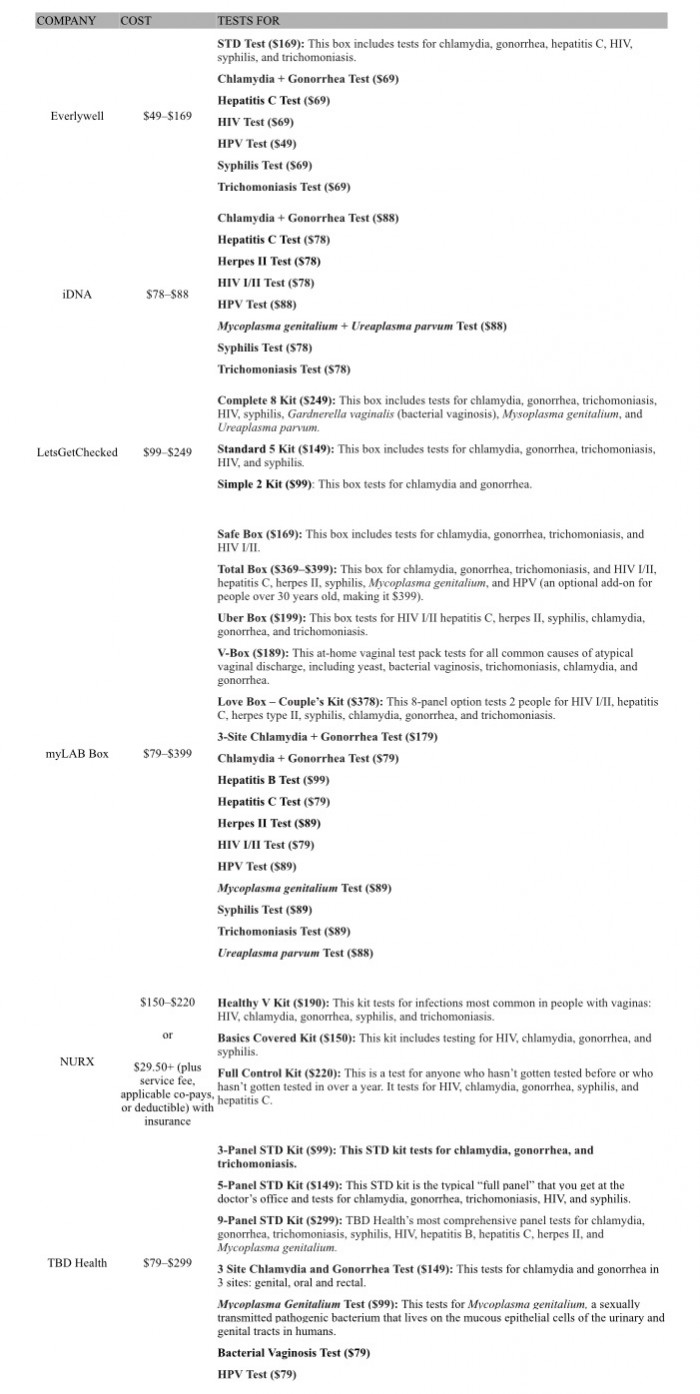
Embarrassment, aversion to doctor visits, or lack of time are common reasons why a significant number of people choose not to undergo testing, reiterated Chen. As a solution, several companies, such as TBD Health, Everlywell, myLAB Box, LetsGetChecked, iDNA, and NURX, now provide an array of at-home testing and treatment options for STIs and STDs.
A Lack of STI Testing in the US
In a national-level study published in the Journal of Adolescent Health, researchers found that most sexually active participants, aged between 15 and 25 years old, had never received an STI test. In the past year, only 11.5% had been tested for an STI, revealing that females were more likely to be tested than males, with 17% of females and 6% of males having been tested. The study also discovered that 42% of young people had not been tested for STIs because they believed they were not at risk despite being sexually active.
Some STIs are asymptomatic and, if left untreated, can lead to numerous health complications, including infertility, increased risk of HIV, pregnancy complications, cancer, chronic pain, or even death, in rare cases. Although the Affordable Care Act (ACA) requires insurance companies to provide free annual screenings for the four most reported STIs — HIV, gonorrhea, syphilis, and chlamydia — it lacks support for many, especially those who need more than one test a year, noted Chen.
“When looking at insurance plans, some of them will cover STI testing only once a year, forcing patients into believing that they should only have one sexual partner a year, which is an inherent value judgment on the kinds of dating, lifestyle, or romantic relationship models people subscribe to,” said Chen.
Benefits of Online Sexual Health Services
Online sexual health services provide convenient at-home testing for STIs and STDs for everyone. Some offer remote consultations with healthcare providers who can diagnose and treat STIs, prescribe medication, and provide follow-up care. Users can order testing kits online, and once they receive their results, they can connect with a healthcare provider through the website for further guidance and treatment.
At-Home STI Testing
Chen notes that at-home testing emphasizes privacy, convenience, and accessibility, with the goal of making sexual health testing and care more accessible to individuals who may be uncomfortable or unable to access traditional healthcare settings.
“Hybrid sexual healthcare platforms make sexual healthcare accessible, affordable, approachable, and sex-positive,” insisted Chen. “The process is very simple — patients receive their kit within 1 or 2 days, and it takes less than 10 minutes to collect the samples needed to run a full STI panel.”
Hybridized sexual healthcare platforms, such as TBD Health, Everlywell, myLAB Box, LetsGetChecked, iDNA, and NURX, offer at-home testing kits for chlamydia, gonorrhea, HIV I/II, syphilis, hepatitis B, hepatitis C, trichomoniasis, herpes simplex II, HPV, Gardnerella vaginalis (bacterial vaginosis), Ureaplasma parvum, and Mycoplasma genitalium, ranging from $29.50+ with insurance to $399.
Chen mentioned that a comprehensive 9-panel STD test is recommended for those who have multiple sex partners or had sexual contact with someone whose STD status is unknown.
Some of the benefits of at-home STI testing include convenience, privacy, early detection, accuracy, and peace of mind, emphasized Chen. For people who are uncomfortable with discussing their sexual health with a doctor or going to a clinic, at-home testing can provide a discreet and accurate way to get screened for STIs.
When asked about the accuracy and specificity of testing samples collected by patients, Chen shared that molecular diagnostics is used to determine the results of the samples processed in their CAP- and CLIA-validated laboratory.
“The samples collected for at-home tests are just as reliable as clinician-collected samples and, in some cases, are more reliable,” she added. “In fact, studies indicate that patients know their body better and can get a more invasive sample.”
For example, a study published in the BMJ found that self-taken vulvovaginal swabs analyzed by nucleic acid amplification tests were significantly more sensitive to detecting gonorrhea than urethral and endocervical cultures taken by a clinician.
When an STI test result is positive, it is important to follow up with a trusted healthcare provider for treatment and follow-up testing. While at-home STI tests can be a useful tool to determine when to seek treatment, they should not replace regular check-ups with a healthcare provider.
“Every set of results that comes through TBD Health is reviewed by a licensed clinician, a nurse practitioner, or a doctor,” Chen highlighted. “Patients are getting personalized high guidance and counseling online — not just a readout from a lab that may be hard to understand for some patients.”
Forming an open channel of communication with healthcare providers is critical to receiving proper sexual healthcare. To help patients easily connect with a trusted and broad-minded healthcare provider, Chen noted that TBD Health is developing a national directory composed of referred specialists that are guaranteed to approach sexual healthcare with positivity and inclusiveness.
Is STI Testing Covered by Health Insurance?
Unfortunately, the answer to this question is not a simple “yes” or “no”, as coverage for STI testing and treatment can vary depending on the type of testing needed and the current health insurance plan.
Many insurance programs cover common STI testing annually as part of routine preventive care, but for those whose insurance plan doesn't cover the cost of STI testing and treatment, there are often low-cost or free options available through public health clinics, community organizations, or government programs that require in-person testing.
The out-of-pocket price range for STD testing and treatment in the US varies from $108 to $600, contingent on the specific STDs being tested, the presence of symptoms, or the need for an examination.
On average, an out-of-pocket STI test for chlamydia, herpes simplex virus II, gonorrhea, syphilis, and trichomoniasis from Planned Parenthood without insurance ranges from $130 to $270, depending on location and a sliding-income scale.
While STD testing with and without insurance can be expensive, at-home STI testing services offer convenient and affordable options by accepting FSA/HSA payment options and may be covered by health insurers in the future.
“Currently, TBD Health is cash pay but can provide superbills, or invoices, for those who want to submit for insurance reimbursement. However, accepting insurance is something that we are actively working on,” reassured Chen.
As more at-home testing companies continue to work toward accommodating insurance coverage to eliminate or lower the cost of STI testing, California has become the first state to require health insurance plans to cover at-home tests for STIs, including HIV, chlamydia, gonorrhea, and syphilis, under Senate Bill (SB) 306.
Senate Bill 306 states that “A health insurance policy issued, amended, renewed, or delivered on or after January 1, 2022, excluding specialized health insurance policies, shall provide coverage for home test kits for sexually transmitted diseases, including any laboratory costs of processing the kit, that are deemed medically necessary or appropriate and ordered directly by an in-network clinician, or furnished through a standing order for patient use based on clinical guidelines and individual patient health needs.”
“Although Governor Newsom mandated health insurers cover at-home STI testing in 2022, there are structural changes that need to happen before the insurance benefit becomes widespread,” admitted Chen. “For example, more Current Procedural Terminology (CPT) codes are needed.”
According to the American Medical Association, a CPT code offers healthcare professionals a uniform language for coding medical services and procedures to streamline reporting and increase accuracy and efficiency. They are also used for administrative management purposes such as claims processing and developing guidelines for medical care review.
Normalizing Testing and Treatment
Sexual health can be stigmatized for a variety of reasons, including cultural, religious, and societal attitudes toward sex and sexuality. Some other common reasons why sexual health is stigmatized include taboos, misinformation, moral judgments, fear of judgment, and gender norms, explained Chen.
Sexual activity can be viewed as immoral or sinful by some individuals or communities, leading to negative attitudes and judgment toward those who are sexually active or have STIs. People may fear judgment or discrimination from others if they disclose their sexual history or STI status, leading to a reluctance to seek testing and treatment. In many societies, there are different expectations and attitudes toward men's and women's sexual behavior, with women often facing greater stigma and judgment for their sexual activity.
Reducing stigma and increasing education and awareness about sexual health can help to improve access to testing and treatment, reduce shame and discrimination, and promote overall sexual health and well-being.
“Sexual health is incredibly important to one’s overall health and well-being. It is certainly not something to be shunted to the side or whispered about — it's something to be celebrated beyond the confines of fertility and reproductive health,” concluded Chen.
