How Continuous Glucose Monitors Have Impacted Chronic Disease Management
Continuous glucose monitors have impacted chronic disease management for patients with diabetes and clinicians by providing additional insight into blood sugar changes.

Source: Getty Images
- Within the past 25 years, continuous glucose monitors have been introduced and integrated into multiple aspects of diabetes care, revolutionizing chronic disease management and positively impacting treatment regimens and lifestyles. The increased data availability has allowed patients and providers better insight into patient health.
Diabetes is a chronic condition that impacts blood sugar levels. According to the CDC, people with type 1 diabetes make little to no insulin and are unable to process sugars in the body. For people with type 2 diabetes, the body can create insulin but uses it poorly.
In a 2021 publication in the Journal of Diabetes Science and Technology, researchers state that between 2000 and 2021, the number of patients in the United States with diabetes mellitus has gone from 11 million to 30 million.
By 2030, the projected prevalence of diabetes mellitus in the US will be 55 million.
Researchers in the publication state, “the World Health Organization estimates that approximately 422 million adults or 8.5% of the world’s population are currently affected, which represents a fourfold increase in less than 40 years.”
Monitoring blood sugar levels is an essential part of managing this chronic illness. It allows patients and their providers to determine what lifestyle or medication changes need to be made. With the prevalence being as high as previously mentioned, accurate and efficient measurements of glucose levels are essential.
Basics of Continuous Glucose Monitors
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), a subset of the NIH, defines continuous glucose monitoring as tracking blood glucose levels — commonly referred to as blood sugar levels — throughout the day without pause.
These devices function as an alternative to traditional blood sugar monitors, which require the patient to collect blood using a lancet and blood sugar strips at several points throughout the day. Unlike continuous glucose monitors (CGM), traditional glucose monitors only measure blood sugar at singular points throughout the day.
A CGM is composed of three vital components: a sensor, transmitter, and receiver.
The CGM sensor is inserted under the skin of the stomach or the arm, and the NIDDK states, “the sensor measures your interstitial glucose level, which is the glucose found in the fluid between the cells. The sensor tests glucose every few minutes. A transmitter wirelessly sends the information to a monitor.”
While CGMs are often used alongside an insulin pump, it is essential to understand the difference between them. While an insulin pump delivers medication, a CGM monitors blood sugar levels.
A Brief History of Development
According to the Journal of Diabetes Science and Technology, the first CGMs were approved in 1999. “In 1999, Minimed marketed the first CGM system that enabled the recording of a patient’s glucose values over a span of three days, which relied on repetitive sensor calibration with a finger stick glucose sample every 6 to 12 hours,” stated researchers in the publication.
Unlike the current monitors, this device did not deliver real-time data to patients or providers. Instead, the data could be downloaded later for analysis.
Five years later, in 2004, the Medtronic Guardian, the first CGM with wireless transmission, was introduced. It wasn’t until 2007 that the three day monitoring period for CGMs was expanded to seven days with the introduction of the Dexcom STS-7.
By 2017, Eversense had introduced a CGM with a 180 day lifespan.
The Journal of Diabetes Science and Technology article provides a timeline of FDA and European approvals of CGMs, which began over two decades ago.
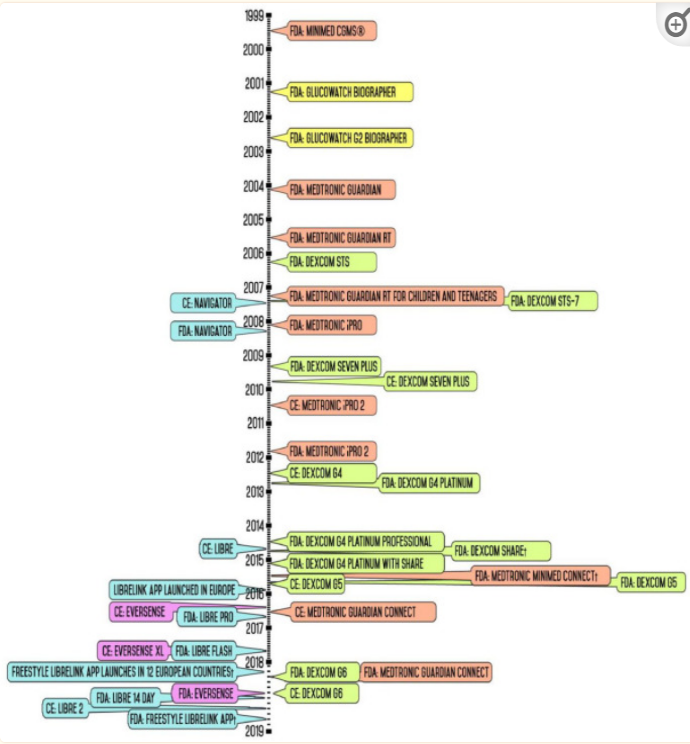
Source: Journal of Diabetes Science and Technology
CGM technology not only has improved the quality of life for many patients but also has been a stepping stone for developing new diabetic care technologies such as artificial pancreas devices.
Types of CGMs
In addition to understanding the basic mechanisms behind CGMs, patients must determine which kind of CGM works best for them.
Below is a picture from UMass Memorial Health comparing the different kinds of available CGMs.
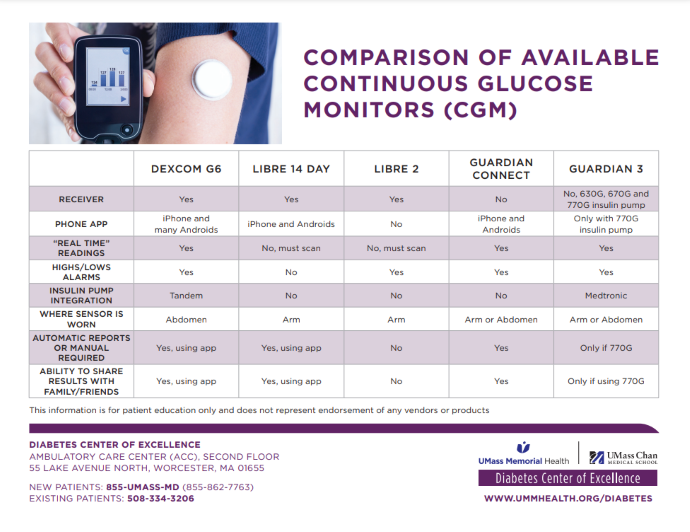
Source: UMass Memorial Health
Benefits and Drawbacks
The primary benefit of CGMs is their ability to collect more real-time data. The Cleveland Clinic states, “fingerstick checks only measure blood glucose at one moment in time. It’s like reading one page of a book. Doing more fingerstick checks gives you more snapshots, which can offer clues to what’s happening with your blood sugar levels."
One drawback of continuous glucose monitors is the potential for misuse. The Cleveland Clinic states that patients using CGMs must learn to insert the sensor correctly, calibrate the device, set alarms as needed, connect the device with a computer or phone, and alter care plans based on collected data.
Many people using these devices require the assistance of a healthcare provider to learn about using the device properly. Additional options include educational classes or individual sessions with a certified diabetes educator.
Despite the initial difficulties of getting the device and learning how to use it, CGMs can provide vital information and alleviate other challenges in managing blood sugar for patients with diabetes.
As mentioned by the Cleveland Clinic and many other healthcare organizations, the data collected by CGMs can give a better overlook of the effects of diabetes. It shows how a patient’s blood sugar is affected continuously before, after, and during meals, exercise, and other essential events, unlike fingerstick monitoring, which can only feasibly show blood sugar changes before and after these events. Theoretically, a patient can opt for a repetitive fingerstick to collect this data; however, that method is unreliable, painful, and costly.
Because a large data set is collected for each patient over the entire day, physicians can use this data alongside patient history to personalize treatment plans.
Another benefit of CGMs is the alerts that can be set for highs and lows. The Cleveland Clinic states, “most CGM devices send an alert when your glucose levels rise or fall a certain amount. With this information, you can make changes quickly. You may be able to treat or prevent highs or lows before they turn into a big problem.”
These alerts can benefit patients unable to monitor their blood sugar on their own effectively.
Regarding the benefits and drawbacks of CGM usage, the Cleveland Clinic says, “learning how to use a CGM device can take time. It’s not a diabetes cure or a quick fix. But it has the potential to help you better understand the disease. A CGM device lets you keep a closer eye on glucose trends (instead of individual glucose numbers). By seeing the bigger picture, you can prevent problems or catch them early on to better manage your health. CGM’s automated, ‘always-on’ setup may give you more freedom, flexibility, and peace of mind. It could also help you focus on other things without worrying about your blood sugar as much.”
Looking Forward
CGM research and development are continuing to build better devices. While this device has drastically impacted and improved the lives of millions of people with diabetes, biotechnology companies are looking to enhance further these devices' accuracy, usability, and longevity.
Providers are encouraged to discuss CGMs as a method of chronic disease management with patients. The decision to use CGMs should be based on multiple factors, including medical history and lifestyle.
