CRISPR Treatment in Clinical Trial for Pediatric Sickle Cell Disease
Recently, the European Hematology Association released clinical trial research with implications for using CRISPR treatment for pediatric sickle cell disease.
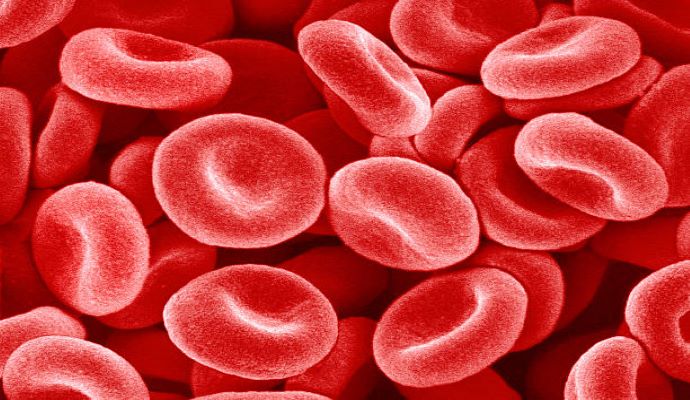
Source: Getty Images
- The European Hematology Association (EHA) recently released results from a clinical trial that implied the potential benefits of using CRISPR treatment to address pediatric sickle cell disease (SCD). CRISPR’s wide variety of applications has made it widely regarded as a leading gene-editing technology.
According to the NIH, in the United States, more than 100,000 people are affected by SCD. That number grows to over two million when looking globally. SCD causes red blood cells to form a crescent rather than their natural disc-like shape. This reduces blood flow and oxygenation to tissues which can have potentially fatal outcomes.
Unfortunately, SCD treatment is limited. While the CDC identifies the most common treatment as symptom management, the only approved “cures” for SCD are bone marrow and stem-cell transplants.
Based on information from Be the Match Bone Marrow Registry, the likelihood of finding a bone marrow transplant depends heavily on ethnic background, with people of African descent having only a 29% chance of finding a match. Unfortunately, 1 in 13 African Americans will be born with the sickle-cell trait.
The recent press releases by Vertex Pharmaceuticals and CRISPR Therapeutics highlight the results of a longitudinal study that focused on using CRISPR to treat transfusion-dependent beta-thalassemia and severe sickle cell disease.
This trial used CRISPR cell therapy to target the erythroid enhancer region of BCL11A of stem cells in patients ranging from 12 to 35. Over the span of several months, patients were monitored for multiple disease-specific factors, including hemoglobin levels, vaso-occlusive crises, transfusions, and adverse events.
The results “further demonstrate the potential of this investigational therapy as a one-time functional cure for patients with transfusion-dependent beta-thalassemia or severe sickle cell disease,” said Carmen Bozic, MD, Executive Vice President, Global Medicines Development and Medical Affairs, and Chief Medical Officer at Vertex in their announcement.
With 2,000 children in the US being born with SCD annually, this new approach could significantly impact early interventions and treatments. Despite CRISPR gene therapies having promising results, there are multiple ethical concerns to consider.
Furthermore, additional research is needed to determine how these therapies could affect a younger population to expand pediatric usage.
The Children’s Hospital of Philadelphia quotes Stephan A. Grupp, MD, PhD, Section Chief of the Cellular Therapy and Transplant Section and Inaugural Director of the Susan S. and Stephen P. Kelly Center for Cancer Immunotherapy at CHOP, who says, “although we must continue to investigate the durability of these results, I am excited about the current data.”
